Abstract
Introduction: Posterior reversible encephalopathy syndrome (PRES) is a novel clinico-radiological syndrome which is characterized by variable symptoms including visual disturbances, headache, vomiting, seizures and altered consciousness, usually accompanied by hypertension. Several cases of immunotherapy-related PRES have been reported as a rare cause of PRES. We present a case of a 52-year-old male who was started on the immunotherapy nivolumab for his esophageal cancer. He came to the hospital with progressive vision loss and was diagnosed with PRES along with optic neuritis.
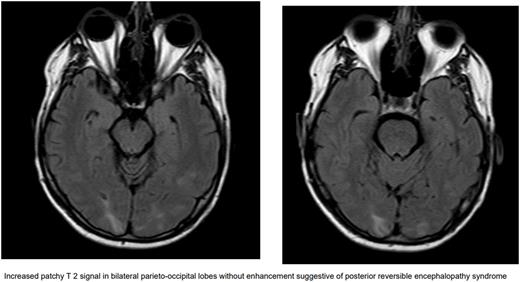
Case Presentation: A 52-year-old male with no significant past medical history presented to the hospital with left sided numbness and spatial recognition issues. A computed tomography (CT) of the head revealed a 3 cm right parietal mass with vasogenic edema later confirmed with a magnetic resonance imaging (MRI) of the brain. He was started on steroids along with 500 mg Keppra twice a day. CT of the chest, abdomen, and pelvis showed multiple hepatic masses and retroperitoneal lymphadenopathy. He had a colonoscopy about a year prior that was unremarkable. He underwent right frontal parietal craniotomy for single brain metastatic lesion. The biopsy of both the brain and liver mass revealed metastatic adenocarcinoma. He was discharged and started on Fluorouracil, Folinic Acid, Oxaliplatin (FOLFOX) chemotherapy as outpatient for possible upper gastrointestinal (GI) cancer. After two cycles of chemotherapy, a positron emission tomography (PET) scan revealed suspected primary esophageal cancer. Though patient had zero PDL-1 biomarker, nivolumab was added to cycle 3 of FOLFOX with the expectation of having a better response early in the disease. He continued to have stereotactic radiosurgery (SRS) along with steroid taper for local control of brain metastasis. Nivolumab was held after cycle 2 as he developed mild headache, fever and elevated lipases. He was found to be hypertensive to 144/85 mmHg. MRI brain showed improving post-surgical changes. On improvement of symptoms, Nivolumab was reintroduced to cycle 6 of FOLFOX. Unfortunately, a week later he developed progressive vision loss more on right eye. He was sent to optometrist who referred patient to emergency room (ER) because of concern for bilateral papilledema. On admission to ER, he was hypertensive to 182/104 and tachycardic to 107 beats per minute. Physical exam was significant for left inferior quadrantanopia more prominent in right eye. CT head was unrevealing for any infarct. MRI of the orbit and brain showed increased patchy T 2 signal in bilateral parieto-occipital lobes without enhancement suggestive of posterior reversible encephalopathy syndrome (PRES) along with right optic neuritis. These findings were attributed to the immunotherapy nivolumab. He was started on a high dose of prednisone, 1mg/kg/day along with 20 mg lisinopril for strict blood pressure control with a goal of 120/80 mmHg. He was discharged with tapering steroids dose and his symptoms improved within 1 week of treatment.
Discussion: Posterior reversible encephalopathy syndrome is a clinico-radiological diagnosis. The underlying pathophysiology involves hypertension and endothelial dysfunction. Hypertension leads to cerebral hyper-perfusion which may cause vascular damage and vasogenic edema leading to blood brain barrier dysfunction. The posterior circulation is the most susceptible to blood pressure changes, thus it is the most common imaging abnormality. PRES frequently develops in the context of cytotoxic medication, immunotherapy, (pre)eclampsia, sepsis, renal disease or autoimmune disorders. MRI is an important diagnostic tool and displays hyperintense lesions in T2-weighted or FLAIR sequences in the parietal-occipital lobes in about 70% of cases but other parts can also be involved. Electroencephalogram (EEG) and lumbar puncture (LP) can be done to rule out other causes. Differentiation is important from an ischemic event as management is different in both cases. Treatment of PRES is symptomatic. Recommendations are to avoid fluctuations in blood pressure with a goal of 130-150/80-100mmHg. If any triggering factor or condition is identified like immunotherapy, it should be avoided or treated accordingly.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal